Navigate the complexities of health insurance lead generation in the post-ACA landscape. This comprehensive guide covers enrollment period strategies, CPL benchmarks, subsidy-eligible targeting, compliance requirements, and the market dynamics that shape this regulated vertical.
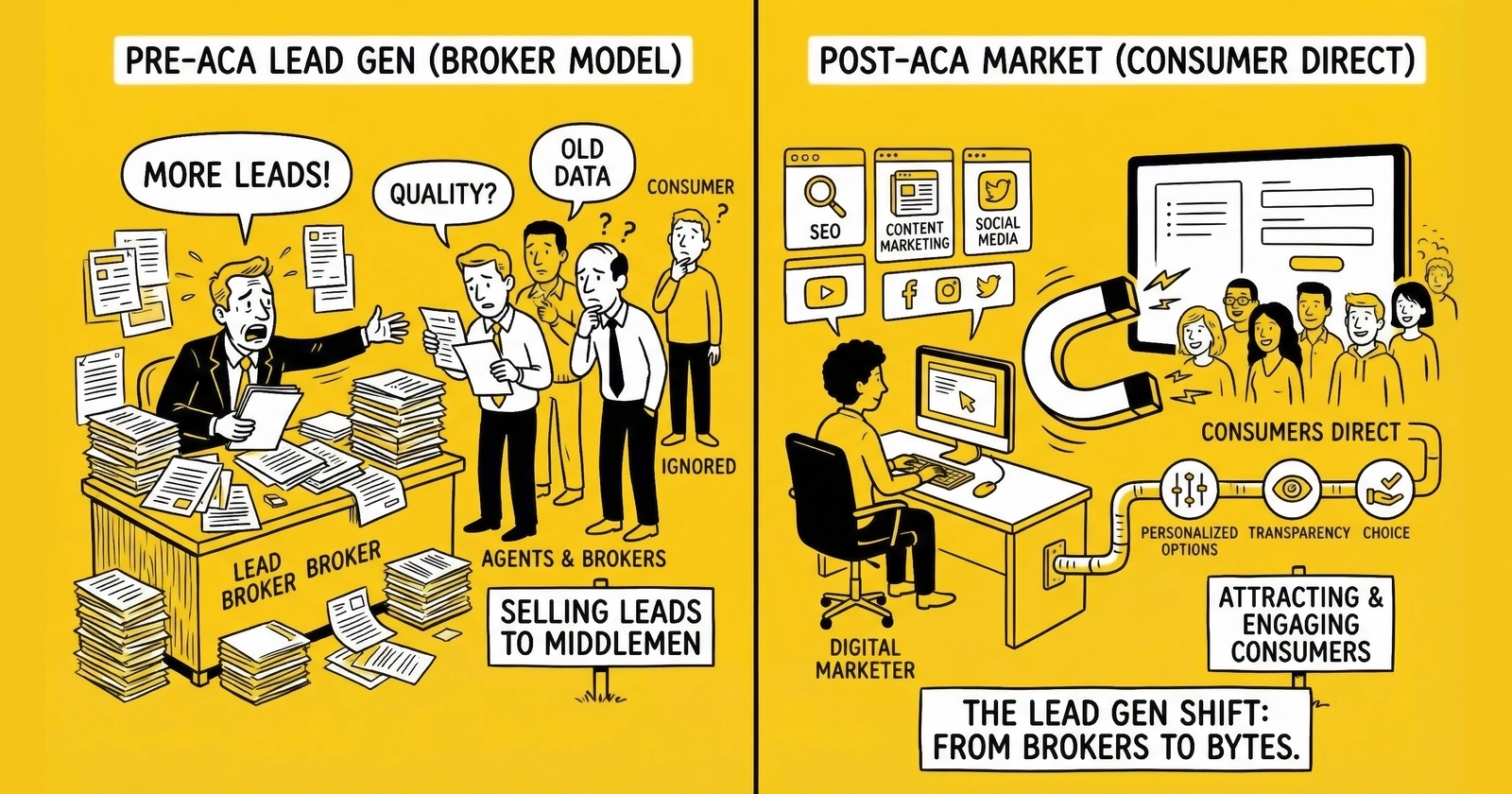
The Affordable Care Act transformed American health insurance. It also created an entirely new lead generation vertical with dynamics unlike any other in the industry.
When the first Healthcare.gov enrollment period launched in 2013, chaos ensued. The website crashed, consumers flooded call centers, and a scramble for market share began that continues to this day. What emerged from that chaos is a multi-billion dollar ecosystem connecting consumers seeking coverage with carriers, brokers, and navigators competing for their attention during compressed enrollment windows.
The Under-65 health insurance market operates under rules that make it fundamentally different from auto, mortgage, or even Medicare lead generation. Annual enrollment periods concentrate demand into weeks rather than months. Subsidy eligibility creates economic segmentation that determines consumer behavior. Special Enrollment Periods triggered by qualifying life events generate year-round opportunity for those who understand the triggers. And regulatory complexity from both federal and state authorities creates compliance requirements that eliminate casual operators.
This guide provides the operational intelligence you need to succeed in health insurance lead generation. Whether you are a lead generator targeting the ACA marketplace, a broker building your book of business, or an agency scaling enrollment operations, you will understand the market dynamics, pricing benchmarks, and compliance frameworks that determine who wins in this vertical.
The Post-ACA Health Insurance Landscape
The Affordable Care Act did not simply reform health insurance. It created an entirely new market structure with enrollment periods, subsidy systems, and regulatory oversight that fundamentally changed how consumers shop for coverage and how lead generators reach them.
Market Size and Structure
The ACA marketplace has grown substantially since its turbulent launch. Enrollment for 2024 coverage reached approximately 21.3 million people through the federal and state marketplaces, a record high reflecting both expanded eligibility and enhanced subsidies. The 2025 Open Enrollment Period pushed this further, with enrollment projections exceeding 22 million.
This growth translated directly into lead generation demand. The health insurance lead market within the Under-65 segment represents an estimated $500 million to $800 million in annual transaction value, depending on how the market boundaries are defined. This figure encompasses direct carrier and broker spending on performance marketing, intermediary transaction values, and affiliated agency volume.
Understanding Market Segments
The market divides into four distinct segments, each with unique characteristics and lead generation dynamics.
The Individual Marketplace, also known as the ACA Exchange, serves consumers purchasing coverage through Healthcare.gov or state-based exchanges, often with Premium Tax Credit subsidies. This segment drives the majority of health insurance lead volume and commands premium pricing during Open Enrollment. For most lead generators, marketplace leads represent the core business opportunity.
Off-Exchange Individual coverage targets consumers purchasing directly from carriers without subsidies. Higher income consumers who do not qualify for Premium Tax Credits sometimes prefer off-exchange plans with different network or benefit structures. These consumers tend to be more price-sensitive and shop more aggressively since they bear the full premium cost.
Short-Term Medical represents limited-duration policies that do not meet ACA requirements but offer lower premiums for healthy consumers willing to accept coverage gaps. Regulatory treatment varies dramatically by state, with California, New York, and New Jersey banning short-term plans entirely while other states allow the federal maximum duration of three years with renewal.
Health Sharing Ministries operate as faith-based cost-sharing programs that are not insurance but serve as ACA alternatives. Lead generation for these programs faces different regulatory requirements than traditional health insurance, and operators must understand the distinction between insurance solicitation and health sharing program marketing.
The Enrollment Period Calendar
Unlike most insurance verticals where consumers can purchase coverage year-round, ACA marketplace enrollment concentrates into defined periods. This calendar creates the most pronounced seasonality in health insurance lead generation.
Open Enrollment Period Dynamics
The annual Open Enrollment Period runs from November 1 through January 15 in most states, though some state exchanges extend deadlines. During OEP, any consumer can enroll in or change marketplace coverage for the following plan year. This 10-11 week window accounts for 60-70% of annual health insurance lead volume.
The OEP creates concentrated demand that spikes CPL, compresses return windows, and requires operational scaling that catches many practitioners unprepared. Lead generators who lack OEP capacity miss the majority of annual opportunity. Lead buyers who lack OEP sales infrastructure cannot absorb available inventory. The mismatch between preparation and opportunity defines who wins and who struggles.
Key OEP dates for the 2025-2026 enrollment cycle begin on November 1, 2025, when Open Enrollment opens. December 15, 2025 marks the deadline for January 1 coverage effective date, creating the year’s highest demand spike. January 15, 2026 closes Open Enrollment for most states, though consumers in state-based exchange states should verify local deadlines.
Special Enrollment Period Triggers
Outside OEP, consumers can only enroll if they experience a Qualifying Life Event that triggers a Special Enrollment Period. The most common SEP triggers fall into several categories that smart lead generators learn to target effectively.
Coverage loss events include job loss, aging off a parent’s plan at 26, divorce ending spousal coverage, and loss of Medicaid or CHIP eligibility. These events create motivated consumers who need coverage quickly and have a clear 60-day enrollment window.
Life changes such as marriage, birth or adoption of a child, and moving to a new coverage area each trigger 60-day SEP windows. These consumers often combine health insurance shopping with other major life decisions, creating cross-selling opportunities for savvy brokers.
Status changes including gaining citizenship or lawful presence, leaving incarceration, and certain income changes affecting subsidy eligibility also qualify. These triggers often require additional documentation but represent reliable year-round lead sources.
SEP leads maintain relatively consistent pricing year-round but require verification of qualifying events. Lead forms that capture qualifying event information command premium pricing because they confirm enrollment eligibility and reduce wasted contact attempts.
The Subsidy Factor
Premium Tax Credits fundamentally reshape health insurance consumer behavior and lead economics. Understanding subsidy dynamics is essential for effective targeting and qualification.
The American Rescue Plan Act enhanced Premium Tax Credits in 2021, and the Inflation Reduction Act extended these enhancements through 2025. These enhanced subsidies eliminated the “subsidy cliff” that previously cut off assistance at 400% of the Federal Poverty Level, allowing higher-income consumers to qualify for credits if benchmark plan premiums exceed 8.5% of household income.
How Subsidies Shape Consumer Behavior
Consumers with substantial subsidy eligibility face dramatically different economics than those paying full price. A consumer eligible for a $400 monthly subsidy reducing their premium from $550 to $150 is highly motivated to enroll and maintain coverage. Their effective cost falls far below market rates, making enrollment an obvious decision with immediate financial benefit.
Consumers at higher income levels who receive minimal subsidies or none at all face full premium costs. These consumers shop more aggressively, consider alternatives like short-term coverage, and may choose to go uninsured if premiums exceed their perceived value. Converting these leads requires different messaging and often produces lower conversion rates.
Targeting Subsidy-Eligible Populations
Lead generators can target subsidy-eligible populations through multiple channels. Income targeting on advertising platforms allows precise audience selection based on household income ranges. Geographic targeting in areas with high uninsured rates concentrates spend where demand exists. Content marketing addressing subsidy eligibility questions attracts consumers actively researching their options. Messaging that emphasizes “$0 premium” or low-cost options resonates with cost-conscious consumers seeking affordable coverage.
Subsidy-eligible leads often convert at higher rates because the economic case for enrollment is clearer. However, targeting very low-income consumers may result in Medicaid eligibility rather than marketplace enrollment, depending on state Medicaid expansion status. Sophisticated practitioners adjust targeting based on state-specific Medicaid thresholds to maximize marketplace-eligible lead flow.
State Market Variations
Health insurance lead generation faces significant state-by-state variation in market dynamics, regulatory requirements, and available products that operators must understand.
State-Based Exchange Considerations
Eighteen states and the District of Columbia operate their own health insurance marketplaces rather than using Healthcare.gov. These states often have different enrollment deadlines, supplemental state subsidies, and distinct regulatory requirements. Major state-based exchanges include Covered California, NY State of Health, Massachusetts Health Connector, Connect for Health Colorado, and Washington Healthplanfinder among others.
Lead generators operating in state-based exchange states must understand state-specific enrollment calendars and may face additional regulatory oversight beyond federal requirements. Some state exchanges extend enrollment deadlines past the federal January 15 date, creating late-OEP opportunities unavailable in Healthcare.gov states.
Medicaid Expansion Impact
States that expanded Medicaid under the ACA cover adults up to 138% FPL through Medicaid rather than the marketplace. In expansion states, leads from very low-income consumers may convert to Medicaid rather than marketplace coverage, affecting lead value for brokers who receive no compensation for Medicaid enrollments.
Ten states have not expanded Medicaid, creating a “coverage gap” where adults below poverty level may not qualify for either Medicaid or marketplace subsidies. Lead generation in these states requires awareness of which consumers can actually obtain coverage, making income-based targeting particularly important.
Short-Term Medical Availability
State regulation of short-term medical plans varies dramatically and directly impacts lead monetization options. California, New York, and New Jersey ban short-term plans entirely. Other states limit duration to 90 days, 6 months, or 12 months. States following federal guidelines allow the maximum duration of three years with renewal options.
Lead generators serving short-term medical buyers must understand state-level availability before accepting leads from restricted states. Generating leads in states where the product cannot legally be sold creates compliance risk and wastes marketing spend.
CPL Benchmarks: What Health Insurance Leads Actually Cost
Lead pricing in health insurance follows predictable patterns based on enrollment period timing, lead quality, and distribution model. These benchmarks reflect 2024-2025 pricing across established intermediaries and direct relationships.
Open Enrollment Period Pricing
OEP creates the year’s highest demand and pricing. Carriers and agencies scale aggressively to capture their share of annual enrollments, driving competition for quality leads.
| Lead Type | OEP CPL Range | Typical OEP CPL | Notes |
|---|---|---|---|
| Shared ACA Leads | $25-50 | $35-45 | 3-5 buyers per lead |
| Exclusive ACA Leads | $55-100 | $70-85 | Single buyer, verified consent |
| Subsidy-Qualified Leads | $65-120 | $80-95 | Income-qualified for PTC |
| Live Transfers | $100-175 | $125-150 | Warm transfer, pre-screened |
OEP pricing runs 20-40% above off-season rates. Early OEP from November 1-30 commands premium pricing as buyers front-load campaigns. Late OEP after the December 15 deadline sees price compression as volume declines and buyers reach enrollment targets.
Special Enrollment Period Pricing
SEP leads maintain relatively consistent pricing year-round, without the seasonal spikes of OEP. However, SEP leads require qualifying event verification that adds value.
| Lead Type | SEP CPL Range | Typical SEP CPL | Notes |
|---|---|---|---|
| Shared SEP Leads | $20-40 | $28-35 | Basic qualifying event capture |
| Exclusive SEP Leads | $45-80 | $55-70 | Single buyer, event documented |
| Event-Verified Leads | $60-100 | $70-85 | Qualifying event confirmed |
| Live Transfers | $85-150 | $100-125 | Year-round availability |
The critical differentiator for SEP leads is qualifying event documentation. Leads that capture specific qualifying event details such as date of job loss, moving date, or marriage date command premium pricing because they confirm enrollment eligibility and enable faster processing.
Pricing by Quality Tier
Within any lead type, quality filtering creates pricing tiers that reflect validation depth and conversion probability.
Basic Tier Economics
Basic tier leads at $25-45 provide minimal qualification beyond contact information. These leads may include unverified income or subsidy eligibility claims and carry higher return rates. Operations with high-volume capacity and strong sales processes can extract value from basic tier leads through aggressive contact cadences and efficient qualification workflows.
Standard Tier Value
Standard tier leads at $45-75 capture income range for subsidy estimation and verify current coverage status. Contact information undergoes validation, and TrustedForm or Jornaya certification comes included. This tier balances cost against qualification depth and serves most buyer requirements effectively.
Premium Tier Quality
Premium tier leads at $75-120 and above capture full income and household information for accurate subsidy calculation. Subsidy eligibility gets estimated and displayed to the consumer during form completion. For SEP leads, qualifying events are documented with dates. Distribution is exclusive with verified consent, and delivery happens in real-time via API integration. Premium buyers pay premium prices for leads that convert at premium rates.
Live Transfer Economics
Live transfers represent the premium tier of health insurance leads. A call center agent screens the consumer for intent, basic qualification, and enrollment eligibility before transferring the warm call to the purchasing agent or agency.
Live transfer pricing of $100-175 reflects the near-certain contact since the consumer is already on the phone and engaged. Pre-qualification confirms shopping intent and basic eligibility before transfer. Immediate engagement starts the sales conversation instantly rather than requiring callback attempts. Higher conversion rates of 15-25% compare favorably to 8-12% for form leads.
The unit economics often favor live transfers despite higher per-lead costs. A $125 live transfer converting at 18% yields $694 cost per enrollment. A $50 form lead converting at 8% yields $625 cost per enrollment. When you factor in follow-up costs, agent time for callbacks, and time-to-enrollment, live transfers may deliver better overall economics for operations with the call handling capacity to absorb them.
Geographic Pricing Variation
Health insurance lead pricing varies by state and region based on competition, coverage options, and consumer demographics.
Premium markets commanding 15-30% above average pricing include Texas with its large uninsured population and active broker market, Florida with significant senior spillover and high marketing spend, California as a large market with strong broker presence, and Georgia with high uninsured rates and active marketplace participation.
Standard markets at baseline pricing include most Midwestern and Mountain states, Mid-Atlantic states outside major metros, and the Pacific Northwest.
Discounted markets at 10-20% below average include states with limited carrier competition, states with dominant state Medicaid programs, and very rural markets with low population density that make lead delivery and conversion challenging.
The Enrollment Period Strategies
Success in health insurance lead generation requires different strategies for OEP, SEP, and year-round operations. Each period has distinct dynamics that shape campaign planning, budget allocation, and operational scaling.
Open Enrollment Period Strategy
OEP is the Super Bowl of health insurance lead generation. The concentrated demand window creates both opportunity and operational challenge that separates prepared operators from those caught scrambling.
Pre-OEP Preparation Requirements
Successful OEP campaigns require months of preparation beginning in August and extending through October. Buyer relationship development means new contracts get signed and pricing gets negotiated before the rush. Technology testing verifies API integrations and load-tests delivery systems under simulated peak conditions. Creative development builds landing pages, writes ad copy, and clears compliance review. Traffic source expansion tests new channels and establishes publisher relationships. Staffing plans complete sales team hiring and training while finalizing schedule coverage for extended hours.
Operators who wait until November to prepare OEP campaigns compete against entrenched competitors with optimized funnels and established buyer relationships. The preparation window determines OEP success more than any single tactical decision during the enrollment period itself.
OEP Campaign Phases
The enrollment period divides into three distinct phases with different characteristics and strategic implications.
Phase 1 covering the Launch period from November 1-15 sees volume ramp as carriers and agencies launch campaigns. CPL often starts high as demand exceeds supply, then stabilizes as more inventory enters the market. Focus during this phase centers on capturing early enrollees who want January 1 effective dates and are motivated to complete enrollment quickly.
Phase 2 representing the Peak period from November 15 through December 15 creates the year’s highest demand period. The December 15 deadline for January 1 coverage drives urgency. Buyers compete aggressively for leads, CPL peaks, and sell-through rates approach 100% for quality inventory. This is the critical revenue window that makes or breaks annual performance.
Phase 3 during the Wind-Down period from December 16 through January 15 sees volume and pricing decline. Consumers who missed the January 1 deadline face February 1 or later effective dates with less urgency. Some buyers reduce spending while others see opportunity in reduced competition. Strategic buyers may find value in late-OEP leads at discounted pricing that still convert at reasonable rates.
OEP Budget Allocation
For operations with annual health insurance lead budgets, OEP should command 50-60% of annual spending distributed across the enrollment calendar.
| Period | Budget Share | Rationale |
|---|---|---|
| Pre-OEP Testing (Sept-Oct) | 5-10% | Refine targeting, test creative |
| Early OEP (Nov 1-30) | 20-25% | Capture early enrollees, optimize campaigns |
| Peak OEP (Dec 1-15) | 25-30% | Maximum investment in highest-demand period |
| Late OEP (Dec 16 - Jan 15) | 10-15% | Capture stragglers at reduced CPL |
| Year-Round SEP | 25-35% | Maintain consistent presence |
Special Enrollment Period Strategy
SEP represents the year-round opportunity that sustains operations between Open Enrollment Periods. Success requires different approaches than OEP, with emphasis on qualifying event targeting and verification.
Qualifying Event Targeting Approaches
The most effective SEP lead generation targets specific qualifying life events rather than broadcasting generic health insurance messages.
Job loss and coverage loss events create highly motivated consumers with clear timelines. Target recently unemployed populations through job search platforms and career transition content. Partner with career transition services and outplacement firms. Develop content marketing addressing COBRA versus marketplace coverage decisions. The 60-day SEP window from coverage loss creates urgency that drives conversion.
Life changes including marriage, birth, and moving create SEP opportunities with different consumer mindsets. Life event targeting on advertising platforms reaches consumers during these transitions. Geographic targeting captures relocation-related SEP volume. Partnership opportunities with wedding services, parenting resources, and moving companies extend reach. The 60-day window from event date provides clear enrollment timeline.
Income changes affect populations experiencing financial transitions. Target seasonal workers gaining or losing employment, gig economy workers with variable income, and recent graduates entering the workforce. These consumers may newly qualify for subsidies or lose existing eligibility, creating enrollment motivation.
SEP Lead Qualification Requirements
SEP leads require qualifying event capture to confirm enrollment eligibility. Effective forms collect qualifying event type to categorize the trigger, event date to confirm SEP window validity, current coverage status to understand consumer situation, and expected effective date needs to match urgency with plan options.
Leads with complete qualifying event information command premium pricing because they confirm the consumer can actually enroll. Incomplete SEP leads may represent consumers outside valid enrollment windows, creating wasted contact attempts and buyer frustration.
Year-Round SEP Budget Rationale
Maintaining consistent SEP presence serves multiple strategic purposes beyond immediate lead revenue. Sustained activity maintains buyer relationships between OEP periods when other generators go quiet. Year-round operations capture ongoing opportunity from life events that happen continuously. Consistent presence builds brand awareness for the next OEP cycle. Testing during slower periods optimizes targeting and creative for the following year’s campaigns.
SEP typically represents 25-35% of annual health insurance lead spend, distributed relatively evenly across months with modest adjustments for seasonal life event patterns like spring wedding season or summer moving activity.
Scaling Operations for Enrollment Periods
The 10-11 week OEP window requires operational scaling that many lead generators underestimate until they experience capacity failures during peak demand.
Lead volume scaling requires traffic acquisition to expand 3-5x during OEP compared to year-round levels. Landing page infrastructure must handle peak loads without degradation. Lead delivery systems must maintain real-time performance under sustained high volume. Quality assurance processes must scale without creating bottlenecks that delay delivery.
Buyer capacity alignment ensures that downstream partners can absorb increased lead flow. Buyers must have staffing to handle the surge, and their capacity constraints become your delivery constraints. SLAs may tighten during OEP with faster delivery requirements. Return policies may change with shorter windows and stricter criteria. Payment terms may accelerate as buyers need faster processing during peak periods.
Technology stress testing before OEP should push all systems at 3-5x normal volume. API integrations that work at 100 leads per hour may fail at 500 leads per hour under sustained load. Database queries that complete in milliseconds may timeout under stress. Discovery of these failures during OEP is too late to fix without losing revenue.
Lead Quality and Qualification Standards
Health insurance leads require specific qualification fields that determine value and conversion probability. Understanding what makes a quality lead enables appropriate pricing and buyer expectation management.
Essential Qualification Fields
Effective health insurance lead capture requires comprehensive data collection across several categories.
Contact Information Standards
Contact information forms the foundation of every lead. Full name should appear as it would on an insurance application. Phone number requires validation for line type and carrier to confirm contactability. Email address needs deliverability verification. Mailing address enables state-specific plan availability determination. ZIP code determines available plans and local pricing.
Enrollment Eligibility Data
Enrollment eligibility fields confirm whether the consumer can actually purchase coverage. Current marketplace coverage status indicates whether this is a new enrollment or plan change. Existing coverage from other sources such as employer or Medicaid affects options. Qualifying life event type for SEP leads establishes enrollment eligibility. Event date confirms the SEP window remains valid. Enrollment period confirmation distinguishes OEP from valid SEP situations.
Household Information
Household information enables subsidy calculation and family plan quoting. Household size directly affects subsidy eligibility thresholds. Number of people needing coverage determines plan configuration. Ages of household members significantly impact premium calculations. Tobacco use status affects rates in states that allow tobacco rating. Estimated annual household income drives the entire subsidy calculation.
Coverage Preferences
Coverage preferences help match consumers with appropriate plans. Preferred coverage start date indicates urgency and timeline. Metal tier interest across Bronze, Silver, Gold, and Platinum options suggests budget and coverage expectations. Doctor and network priorities reveal switching concerns. Prescription medication needs identify formulary requirements. Monthly premium budget establishes affordability parameters.
Subsidy Qualification Details
Leads that capture sufficient information to estimate subsidy eligibility command premium pricing. The subsidy determination requires household income, household size, tax filing status which affects income calculation, ages of enrollees, and geographic location since benchmark plans vary by county.
Forms that calculate and display estimated subsidies to consumers often see higher completion rates because consumers understand their potential savings immediately. However, these calculations require regular updates as benchmark premiums change annually and FPL thresholds adjust.
Quality Indicators and Red Flags
Recognizing quality signals and warning signs enables appropriate lead valuation and routing decisions.
Positive Quality Indicators
Strong leads demonstrate engagement and authenticity through multiple signals. Complete household information shows commitment to the process. Realistic income figures that avoid round numbers or threshold-hitting values suggest honest reporting. Specific qualifying event details with precise dates confirm legitimate SEP eligibility. Stated doctor or network preferences indicate genuine shopping intent. Multi-step form completion demonstrates willingness to invest time. Reasonable completion time neither too fast nor too slow suggests human engagement. TrustedForm certification with replay available provides verification capability.
Warning Signs Requiring Investigation
Several patterns indicate potential quality issues requiring scrutiny. Missing or generic phone numbers reduce contactability. Disposable or temporary email addresses suggest low commitment. Inconsistent household information indicates carelessness or fabrication. Qualifying event dates outside valid 60-day windows mean the consumer cannot actually enroll. Completion time under 30 seconds strongly suggests fraud or bot activity. Multiple submissions from same IP address indicate systematic manipulation. Income figures landing exactly at subsidy thresholds suggest gaming rather than accurate reporting.
Return Rate Benchmarks
Return rates measure the percentage of leads rejected by buyers post-purchase. Industry benchmarks for health insurance provide performance standards.
| Lead Type | Acceptable Return Rate | Action Threshold |
|---|---|---|
| Exclusive OEP | 8-12% | Investigate at 15%+ |
| Shared OEP | 10-15% | Investigate at 18%+ |
| SEP Leads | 10-14% | Investigate at 17%+ |
| Live Transfers | 5-10% | Investigate at 12%+ |
Return rates above these thresholds indicate quality issues requiring investigation. Common causes include duplicate leads appearing across buyers, invalid contact information that fails verification, leads outside enrollment windows that cannot convert, and qualification misrepresentation discovered during sales contact.
Compliance Requirements and Regulatory Framework
Health insurance lead generation operates under multiple overlapping regulatory frameworks. Federal ACA regulations, state insurance laws, and TCPA requirements create compliance complexity that eliminates casual operators while protecting those who invest in proper infrastructure.
Federal ACA Compliance
The Affordable Care Act and its implementing regulations create specific requirements for health insurance marketing that operators must understand.
Qualified Health Plan Marketing Standards
Marketing ACA-compliant plans through the marketplace requires attention to CMS guidelines across multiple dimensions. Factual accuracy in plan descriptions prevents misleading consumers about coverage. Clear identification of coverage limitations avoids surprise denials. Appropriate use of plan names and carrier branding respects trademark and regulatory requirements. Accurate representation of premium amounts and subsidies builds trust and reduces complaints. Disclosure of enrollment period limitations ensures consumers understand when they can act.
Navigator and Counselor Requirements
Organizations assisting consumers with marketplace enrollment face specific regulatory requirements as Navigators or Certified Application Counselors. Lead generators selling to navigators or CACs should understand buyer compliance obligations to ensure lead quality meets their standards and avoid creating downstream compliance problems.
Short-Term Plan Disclosure Obligations
Federal regulations require specific disclosures for short-term limited-duration insurance that lead generators should understand. Required statements explain that coverage does not meet ACA requirements, describe potential coverage gaps compared to ACA plans, provide notice about limited consumer protections, and address pre-existing condition limitations. Lead generators serving short-term medical buyers should verify that buyers provide required disclosures and consider whether landing page content triggers disclosure obligations.
TCPA Compliance
The Telephone Consumer Protection Act governs contact methods for health insurance leads as it does all lead generation verticals, with substantial penalty exposure for violations.
Prior Express Written Consent Requirements
For autodialed calls or texts to health insurance leads, consent must be clear and conspicuous in presentation. Sellers authorized to call must be specifically identified in the disclosure. Consent cannot be a condition of purchase or service. Documentation of consent must be captured and retained for potential disputes.
One-to-One Consent Evolution
Though the FCC’s one-to-one consent rule was vacated by the Eleventh Circuit in January 2025 and subsequently repealed, industry best practice continues to favor identifying specific parties in consent disclosures. Many sophisticated buyers require one-to-one consent documentation regardless of the rule’s status, making it a practical requirement driven by buyer standards rather than regulatory mandate.
Documentation Best Practices
Robust consent documentation requires implementing TrustedForm or Jornaya certificate capture for independent verification. Record IP address, timestamp, and user agent for each submission. Capture the exact consent language displayed to the consumer. Retain all documentation for 5+ years to cover potential litigation timelines. Enable certificate replay capability for dispute resolution and defense preparation.
TCPA Penalty Exposure
TCPA violations carry $500-$1,500 per violation, with class actions creating catastrophic exposure for non-compliant operations. In 2024, 2,788 TCPA cases were filed, representing a 67% increase from 2023. Average settlements exceed $6.6 million. Understanding the full TCPA compliance landscape is essential for health insurance operations. Health insurance leads, with their high volume during OEP creating concentrated call activity, present substantial exposure for operations without proper consent infrastructure.
State Insurance Regulations
Health insurance marketing faces state-specific requirements that vary by jurisdiction and create a patchwork of compliance obligations.
Licensing Boundary Considerations
Most states do not require lead generators to hold insurance producer licenses for pure lead generation activities that stop at information capture. However, the line between lead generation and insurance solicitation can blur in ways that trigger licensing requirements. Forms that provide quotes or rate estimates may cross into licensed activity. Recommendations of specific carriers or plans may constitute solicitation requiring licensure. Compensation structures tied to enrollment outcomes rather than lead delivery raise licensing questions. Practitioners whose activities extend beyond basic information capture should consult with insurance licensing counsel to confirm their regulatory status.
State Advertising Requirements
Many states regulate insurance advertising with specific requirements including disclaimers about coverage limitations, carrier identification and approval requirements for advertisements, prohibition of misleading benefit descriptions, and rate accuracy and substantiation requirements. Lead generators whose landing pages discuss specific coverage features or pricing should verify compliance with applicable state requirements rather than assuming federal compliance suffices.
State-Based Exchange Additions
States operating their own health insurance marketplaces may impose additional requirements on marketing and lead generation including certified agent requirements for marketplace enrollment assistance, additional disclosure requirements beyond federal standards, specific enrollment process rules, and enhanced consumer protection regulations. Operating in state-based exchange states requires understanding these incremental obligations.
Buyer Relationships and Distribution
Health insurance lead distribution involves multiple buyer types with different requirements, economics, and relationship dynamics that shape strategic choices.
Carrier Direct Relationships
Major health insurance carriers including UnitedHealthcare, Anthem/Elevance, Cigna, Aetna, Molina, and Centene maintain internal acquisition operations and work with external lead generators.
Working with carriers requires meeting demanding standards. Volume commitments often start at 1,000+ leads monthly minimum to justify integration investment. Quality standards demand strict validation, documented consent, and low return thresholds below 10%. Technology integration means real-time API delivery with ping/post capability for dynamic routing. Compliance verification ensures consent documentation meets carrier legal requirements. Geographic coverage specifications define state and county requirements based on plan availability.
Carrier relationships offer significant advantages including premium pricing for quality leads, stable and predictable demand, clear quality specifications that enable optimization, and professional contracting with reliable payment. The challenges include long sales cycles of 3-6 months to establish initial relationships, demanding SLAs with financial penalties for performance failures, concentrated risk if a major relationship ends, and procurement pressure pushing for pricing concessions.
Broker and Agency Relationships
Independent brokers, General Agencies, and marketing organizations purchase leads to grow their enrollment books with different characteristics than carrier relationships.
Broker buyers typically purchase 50-500 leads monthly per agent or agency, smaller individual volumes than carriers. Technology requirements focus on basic CRM integration or portal access rather than sophisticated API connections. Quality expectations emphasize higher value per-lead with strong preference for exclusivity. Pricing often runs higher per-lead than carrier direct relationships. The relationship orientation favors partnership approaches with long-term focus.
Broker advantages include faster sales cycles measured in weeks rather than months, relationship-based loyalty that persists across market changes, flexibility in lead specifications and delivery requirements, and diversification across many buyers reducing concentration risk.
Broker challenges include smaller individual volume requirements that fragment operations, increased support and communication needs, payment variability with some slow-pay situations, and turnover as agents enter and exit the market requiring ongoing relationship development.
Lead Aggregators and Networks
Lead aggregators purchase from multiple generators and resell to carrier and broker networks. Examples include HealthMarkets, SelectQuote, and various regional operations that connect supply with demand.
Aggregators serve a consolidation function, bringing together supply from multiple generators into unified distribution. They normalize quality and delivery standards across diverse sources. Distribution reaches broad buyer networks that individual generators might not access directly. Quality assurance and fraud detection services add value beyond simple lead routing.
Working with aggregators means lower per-lead revenue compared to direct relationships but higher volume potential. Feedback comes less directly since aggregators mediate buyer communication. Standardized quality requirements simplify compliance but limit differentiation. Payment cycles may move faster due to aggregator cash flow advantages.
Distribution Model Selection
The optimal distribution model depends on operational capabilities and strategic objectives.
Direct carrier relationships work best for operators with high volume capacity, sophisticated technology infrastructure, and long-term strategic focus willing to invest in relationship development. The challenges of long sales cycles, demanding requirements, and concentration risk suit organizations with staying power.
Broker networks fit operators seeking relationship-based business models, geographic specialization, or niche vertical focus. Fragmented demand, varied payment practices, and support requirements suit organizations comfortable with higher-touch operations.
Aggregator partnerships serve operators prioritizing volume and simplicity over per-lead revenue maximization. Lower margins, less direct feedback, and commoditization pressure suit organizations focused on scale efficiency.
The hybrid approach that most successful operations employ diversifies across buyer types. Carrier relationships provide stability and premium pricing anchors. Broker networks offer relationship depth and flexibility. Aggregator volume ensures scale and simplicity for overflow capacity. Balancing across buyer types optimizes both revenue and risk.
Technology and Operations
Effective health insurance lead generation requires purpose-built technology infrastructure that handles enrollment period scaling, compliance documentation, and buyer integration.
Lead Capture Technology
Health insurance lead capture presents unique challenges requiring thoughtful form design and integration choices.
Form Design Principles
Health insurance forms must balance qualification depth against completion rates. Multi-step forms typically outperform single-page forms for complex qualification requirements. A typical progression moves from contact information and ZIP code in Step 1 through household size and income range in Step 2, current coverage status and qualifying events in Step 3, coverage preferences and timeline in Step 4, and finally consent and submission in Step 5.
Progress indicators showing completion percentage and field validation providing immediate feedback reduce abandonment. Mobile optimization is essential with 60%+ of health insurance leads originating from mobile devices, making touch-friendly interfaces and streamlined input fields critical for conversion.
Subsidy Calculator Integration
Forms that estimate subsidy eligibility during completion often see higher conversion rates as consumers understand their potential savings. Integration options include Healthcare.gov API integration which has limited availability, third-party subsidy calculation services that maintain current data, and custom calculators built on FPL guidelines with local benchmark data.
Regardless of approach, keeping calculators current requires annual updates for benchmark premium changes and FPL adjustments. Outdated calculations create consumer confusion and compliance risk.
Consent Documentation Systems
TCPA compliance requires robust consent capture and documentation through specialized services.
TrustedForm from ActiveProspect provides independent verification of consent through JavaScript deployment on lead capture forms that enables real-time session recording. Certificate generation with unique identifiers creates auditable records. Visual replay of consumer interaction demonstrates what the consumer saw and did. Retention options extending to 5 years cover potential litigation timelines.
Jornaya LeadiD from Verisk provides consent documentation plus behavioral intelligence. LeadiD token generation per submission creates unique identifiers. TCPA Guardian consent verification confirms compliant capture. Consumer journey tracking across publishers reveals shopping patterns. Evidence packages support litigation defense when needed.
Consent language on health insurance forms should identify parties authorized to contact the consumer, specify contact methods including calls, texts, and email, note use of automated technology for outbound contact, confirm consent is not required for purchase, and meet clear and conspicuous presentation standards for visibility and comprehension.
Lead Delivery and Distribution
Modern buyers increasingly require real-time delivery via API integration rather than batch file transfers.
Real-time API delivery achieves sub-second lead posting for immediate buyer access. Immediate acceptance or rejection responses enable rapid routing decisions. Field-level validation before acceptance catches data quality issues. Dynamic pricing based on lead characteristics optimizes revenue.
Ping/post technology enables sophisticated distribution for shared leads or buyer-based routing. The ping phase sends partial data to potential buyers for bid or acceptance decisions. The post phase delivers full data to winning buyers after acceptance confirmation. This approach enables real-time price optimization and supports both exclusive and multi-buyer distribution models.
Lead management platforms purpose-built for performance marketing such as boberdoo, LeadsPedia, and Phonexa provide multi-source lead ingestion, real-time validation and enrichment, buyer integration and routing logic, return processing and reconciliation workflows, and reporting and analytics dashboards.
Quality Assurance Systems
Maintaining lead quality requires both real-time and post-submission verification processes.
Real-time validation before lead acceptance includes phone validation through carrier lookup, line type identification, and connection status verification. Email validation checks syntax, domain validity, and deliverability indicators. Address verification uses USPS standardization and deliverability confirmation. Duplicate detection compares against internal databases. Fraud scoring evaluates velocity patterns and behavioral indicators.
Post-submission verification after lead capture includes TrustedForm certificate claim and review, consent language verification against requirements, completion time analysis for anomalies, IP and device fingerprinting review for patterns, and cross-submission pattern detection for systematic issues.
Competitive Dynamics and Market Position
The health insurance lead market features distinct competitive dynamics that shape strategic positioning for both generators and buyers.
The Major Players
Understanding the competitive landscape helps identify opportunities and avoid head-to-head battles with better-resourced competitors.
Large lead aggregators dominate volume in health insurance leads. HealthMarkets operates as a major national player with established carrier relationships. SelectQuote trades publicly and maintains significant health insurance presence alongside its Medicare business. GoHealth focuses primarily on Medicare but continues expanding into Under-65 markets. eHealth operates as a publicly traded marketplace and lead operation with integrated enrollment capabilities.
These aggregators combine proprietary lead generation with third-party purchasing, creating both competition and buyer relationships for independent generators. Understanding whether a potential partner competes with or complements your market position guides relationship decisions.
Insurance technology platforms have entered health insurance lead generation as both competitors and potential partners. Oscar Health emphasizes direct-to-consumer acquisition. Clover Health deploys technology-enabled distribution strategies. Bright Health pursues market-based acquisition approaches. These companies may be lead buyers, direct competitors, or strategic partners depending on your market position and their current priorities.
Digital marketing agencies specializing in insurance marketing generate significant health insurance lead volume through paid search campaigns on Google and Bing, social media advertising on Facebook and Instagram, native advertising through Taboola and Outbrain, and content marketing with SEO strategies. Many agencies both generate leads internally and purchase from third parties to meet client demand, creating dual relationship opportunities.
Competitive Positioning Strategies
Several positioning approaches enable sustainable competitive advantage in health insurance leads.
Vertical Specialization
Focusing on specific health insurance segments enables deeper expertise and more efficient operations. ACA marketplace exclusivity concentrates all resources on the largest segment. Short-term medical specialization serves buyers with specific product needs. Individual market focus in specific states builds regional expertise. Subsidy-eligible population targeting serves the highest-converting consumer segment.
Quality Differentiation
Competing on quality rather than price commands premium positioning. Premium consent documentation exceeds minimum requirements. Enhanced validation and verification reduces buyer risk. Lower return rates demonstrate consistent quality. Exclusive distribution provides competitive advantage for buyers. Quality-focused positioning attracts sophisticated buyers willing to pay for performance.
Technology Advantage
Leading on operational capability creates switching costs that protect buyer relationships. Real-time delivery with sub-second posting demonstrates infrastructure investment. Advanced fraud detection reduces buyer exposure. Seamless buyer integration minimizes implementation burden. Superior reporting and transparency builds trust through visibility.
Geographic Focus
Concentrating on specific markets enables relationship density and deep market knowledge. State-based exchange expertise requires specialized understanding. Regional carrier relationships create exclusive buyer access. Local broker networks provide distribution advantages. Market-specific compliance knowledge reduces risk exposure.
Frequently Asked Questions
What is the difference between ACA marketplace leads and off-exchange leads?
ACA marketplace leads are for consumers enrolling through Healthcare.gov or state-based exchanges, often with Premium Tax Credit subsidies. Off-exchange leads are for consumers purchasing directly from carriers without subsidies. Marketplace leads typically have higher conversion rates because subsidies make coverage more affordable, but off-exchange leads may have higher lifetime value for brokers due to direct commission relationships. Pricing is similar, but qualification requirements differ based on subsidy eligibility.
How much do health insurance leads cost during Open Enrollment?
During Open Enrollment Period (November 1 - January 15), health insurance leads typically cost $35-45 for shared leads, $70-85 for exclusive leads, and $125-150 for live transfers. This represents a 20-40% premium over off-season pricing. Early OEP (November) commands highest pricing, while late OEP (post-December 15) often sees price compression as buyers reach enrollment targets.
Can I generate health insurance leads year-round?
Yes, through Special Enrollment Periods triggered by qualifying life events. Consumers who experience job loss, marriage, birth/adoption, moving, or other qualifying events can enroll outside Open Enrollment. SEP leads require documentation of the qualifying event and typically price at $28-35 for shared leads and $55-70 for exclusive leads. Year-round SEP operations provide consistent revenue between Open Enrollment periods.
What qualifying events trigger Special Enrollment Periods?
Common qualifying events include: losing other health coverage (job loss, aging off parent’s plan, divorce), moving to a new coverage area, getting married, having or adopting a child, gaining citizenship or lawful presence, leaving incarceration, becoming eligible for Medicaid or CHIP, and certain income changes affecting subsidy eligibility. Each event triggers a 60-day enrollment window. Lead forms should capture the specific event type and date to confirm eligibility.
How do subsidy calculations affect health insurance lead value?
Leads from subsidy-eligible consumers often convert at higher rates because Premium Tax Credits make coverage affordable. Consumers eligible for substantial subsidies may pay $50-150 monthly for coverage that costs $400-600 at full price. Lead forms that capture household income and size enable subsidy estimation, adding value for buyers. Subsidy-qualified leads typically command 15-25% pricing premiums over unqualified leads.
What TCPA requirements apply to health insurance leads?
TCPA requires Prior Express Written Consent before autodialed calls or texts to health insurance leads. Consent must be clear and conspicuous, identify parties authorized to call, and not be a condition of purchase. Document consent with TrustedForm or Jornaya certificates, capturing timestamps, IP addresses, and exact consent language. Violations carry $500-$1,500 per call, with class actions averaging $6.6 million in settlements.
Should I work with carriers, brokers, or aggregators for health insurance leads?
The optimal approach depends on your scale and capabilities. Carrier relationships offer stability and premium pricing but require high volume (1,000+ leads monthly) and long sales cycles (3-6 months). Broker relationships provide flexibility and higher per-lead pricing but fragment demand across many buyers. Aggregators offer volume and simplicity but lower margins. Most successful operations diversify across buyer types for stability and optimization flexibility.
What conversion rates should I expect from health insurance leads?
Industry benchmarks show 45-55% contact rates and 10-15% conversion rates for fresh leads during Open Enrollment. Exclusive leads convert 40-60% higher than shared leads. Live transfers convert at 15-25%. SEP leads may show slightly lower conversion rates due to qualifying event verification requirements. Speed-to-contact significantly impacts results, with sub-minute response improving conversion by up to 391%.
How do state-based exchanges affect health insurance lead generation?
Eighteen states plus DC operate their own health insurance marketplaces with different enrollment deadlines and requirements than Healthcare.gov states. Lead generators must understand state-specific calendars (some extend past January 15), certified agent requirements, and additional disclosure obligations. State-based exchange leads may require state-specific buyer relationships and compliance processes.
What technology is essential for health insurance lead generation?
Essential technology includes: multi-step lead capture forms with mobile optimization, TrustedForm or Jornaya consent documentation, real-time phone and email validation, subsidy calculator integration, API-based lead delivery, duplicate detection, fraud scoring, and lead management platform integration. OEP requires stress-testing all systems at 3-5x normal volume to ensure performance under peak load.
Key Takeaways
-
The ACA marketplace drives a $500-800 million annual health insurance lead market, with Open Enrollment Period (November 1 - January 15) accounting for 60-70% of annual volume and commanding 20-40% pricing premiums.
-
OEP pricing benchmarks for 2024-2025: Shared leads at $35-45, exclusive leads at $70-85, and live transfers at $125-150. SEP leads maintain steadier pricing at $28-35 (shared) and $55-70 (exclusive) year-round.
-
Subsidy eligibility fundamentally shapes consumer behavior. Enhanced Premium Tax Credits through 2025 make coverage affordable for millions. Subsidy-qualified leads convert at higher rates and command 15-25% pricing premiums.
-
Special Enrollment Periods provide year-round opportunity for consumers experiencing qualifying life events. SEP leads require event documentation but maintain consistent demand and pricing between OEP windows.
-
State variation is significant. Eighteen states operate independent marketplaces with different deadlines. Medicaid expansion status affects lead value. Short-term medical availability varies dramatically by state.
-
TCPA compliance is non-negotiable. With 2,788 cases filed in 2024 and average settlements exceeding $6.6 million, TrustedForm or Jornaya certification is essential infrastructure for health insurance lead operations.
-
Speed-to-contact determines conversion success. Leads contacted within 60 seconds convert up to 391% higher than those contacted at 5+ minutes. OEP’s compressed timeline makes rapid response even more critical.
-
Diversify buyer relationships across carriers, brokers, and aggregators. Carrier relationships provide stability and premium pricing; broker networks offer flexibility and relationship depth; aggregators provide volume and operational simplicity.
-
Prepare for OEP months in advance. Buyer relationships, technology integration, creative development, and operational scaling require 3-4 months of preparation. Practitioners who wait until November compete against entrenched competitors with optimized systems.
Sources
- CMS Marketplace Products Statistics - Official Centers for Medicare & Medicaid Services enrollment data and marketplace statistics
- Healthcare.gov: Affordable Care Act Overview - Official federal marketplace platform and ACA coverage information
- Healthcare.gov: Special Enrollment Periods - Official qualifying life events and SEP eligibility guidelines
- KFF State Marketplace Enrollment Data - Comprehensive state-by-state ACA marketplace enrollment statistics
- KFF Health Reform Resources - Research and analysis on ACA implementation and policy developments
- KFF Medicaid Resources - State Medicaid expansion status and enrollment data
- CMS Newsroom - Official CMS announcements on enrollment periods and marketplace updates
- FCC TCPA Consumer Guide - Federal telemarketing regulations affecting lead generation
Statistics and pricing benchmarks current as of late 2025. Market conditions, subsidy policies, and regulatory requirements change annually. Verify current data before making significant investment decisions. Enhanced Premium Tax Credits are currently authorized through 2025; future policy changes may affect subsidy availability and consumer behavior.