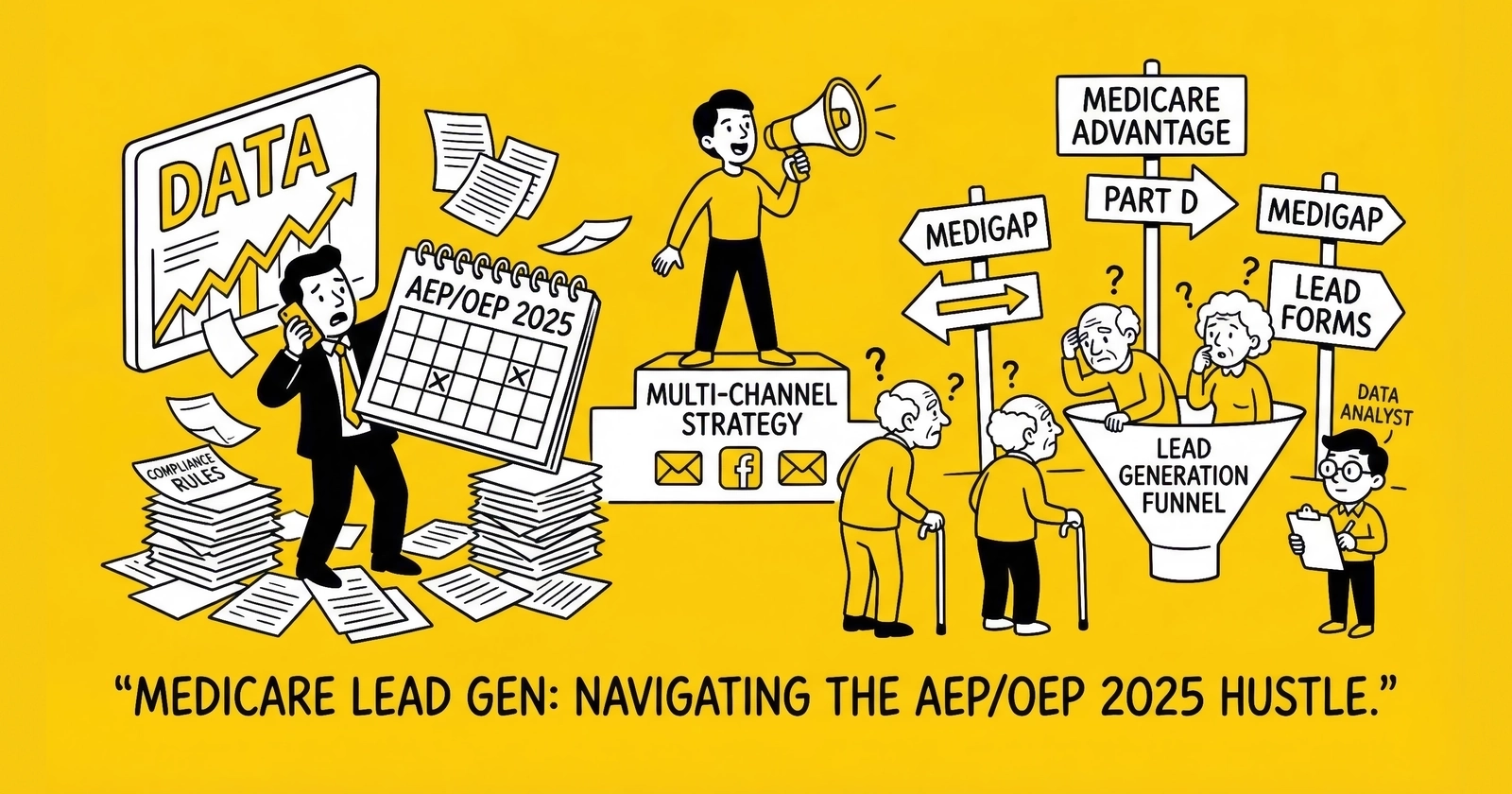
The most heavily regulated lead vertical in America demands precision in timing, compliance, and senior demographic engagement. Master Medicare enrollment periods or watch your operation become a liability.
Medicare represents the intersection of massive demographic opportunity and regulatory complexity that separates sophisticated practitioners from those facing CMS enforcement actions. With 67 million Americans enrolled and approximately 11,000 people turning 65 every day, demand for qualified Medicare leads remains constant. The challenge is not finding interested consumers. The challenge is generating leads that comply with CMS requirements, convert to enrollments, and produce sustainable relationships with carriers and Field Marketing Organizations.
Those who succeed in Medicare lead generation understand three realities their competitors miss: enrollment periods create concentrated windows where 60-70% of annual value materializes, CMS compliance requirements exceed TCPA standards by a considerable margin, and the senior demographic requires fundamentally different engagement approaches than younger consumers in auto insurance or mortgage verticals.
This guide covers the complete Medicare lead generation landscape: enrollment period strategy, CMS regulatory requirements, CPL benchmarks by lead type, carrier and FMO relationships, T65 targeting strategies, and the compliance infrastructure that protects your operation from Civil Monetary Penalties reaching $100,000 or more per violation.
Understanding Medicare Enrollment Periods
Medicare enrollment periods form the foundation of every successful Medicare lead generation strategy. Unlike verticals where demand fluctuates with economic conditions or seasonal patterns, Medicare lead demand follows a rigid calendar defined by the Centers for Medicare and Medicaid Services.
Three primary enrollment periods determine when beneficiaries can enroll in or change Medicare coverage. Each period has different rules, different buyer demand, and dramatically different economics for lead generators.
Annual Enrollment Period: October 15 Through December 7
The Annual Enrollment Period represents the Super Bowl of Medicare lead generation. During these 54 days, Medicare beneficiaries can make nearly any coverage change:
- Switch from Original Medicare to Medicare Advantage
- Switch between Medicare Advantage plans
- Add, drop, or change Part D prescription drug coverage
- Return to Original Medicare from Medicare Advantage with a standalone Part D plan
- Change Medicare Advantage plans with different benefit structures
The AEP accounts for approximately 60-70% of annual Medicare lead value. Every carrier, every FMO, and every independent agent concentrates acquisition efforts in this window. This creates intense competition for consumer attention and corresponding pressure on lead economics.
AEP Lead Economics in Practice
CPLs during AEP run 30-50% above year-round averages. A Medicare Advantage lead that costs $40-55 in July might command $60-85 during peak AEP weeks. Exclusive leads with full qualification regularly exceed $100 during the October 15-November 15 window when buyer urgency peaks.
The math justifies these premiums. Medicare Advantage plans pay agents $694 for initial enrollments in 2026 in most states (the CMS-established national compensation amount, with higher rates of $781 for CT/PA/DC and $864 for CA/NJ), with renewal commissions of approximately $347 continuing annually. An $80 lead that converts at 10% yields an effective cost per acquisition of $800. Against multi-year commission streams that can exceed $2,500-$3,000 per enrolled beneficiary, the acquisition investment makes sense.
Sell-through rates improve dramatically during AEP. Leads that might sell to 60-75% of available buyers during off-season periods achieve 85-95% sell-through during AEP because buyers are aggressively filling capacity before December 7.
AEP Operational Considerations
Budget allocation matters. By November 15, approximately 60% of enrollment decisions have been made. Practitioners who exhaust budgets by mid-October miss the highest-intent portion of the window. Sophisticated operations front-load spending October 15-31 when consumer shopping peaks, then adjust based on buyer feedback and capacity signals.
Creative fatigue accelerates during AEP. Consumers see Medicare messaging across television, radio, digital advertising, direct mail, and community events. Standing out requires creative refresh every 10-14 days rather than the 30-45 day cycles that work during lower-competition periods. Landing page testing should continue throughout AEP, not pause due to volume pressure.
CMS creative approval timelines constrain AEP preparation. Marketing materials used by Third-Party Marketing Organizations must be submitted to and approved by CMS before use. The approval process typically requires 30-45 days, meaning AEP creative development must begin in late August to ensure materials are approved before October 15.
Open Enrollment Period: January 1 Through March 31
The Open Enrollment Period serves a narrower purpose than AEP. During OEP, only beneficiaries already enrolled in Medicare Advantage plans can make changes:
- Switch to a different Medicare Advantage plan
- Drop Medicare Advantage and return to Original Medicare with a standalone Part D plan
OEP does not allow beneficiaries to switch from Original Medicare to Medicare Advantage, add Part D coverage if not currently enrolled, or make changes to Medicare Supplement policies. This limitation substantially reduces the addressable market compared to AEP.
OEP Lead Economics
CPLs during OEP typically run 60-75% of AEP peaks but 15-25% above year-round averages. Lead pricing of $50-70 for qualified Medicare Advantage leads is common, compared to $70-100 during AEP and $40-55 during off-season periods.
Buyer demand during OEP is moderate. Carriers still need leads to fill capacity, but without the urgency that characterizes AEP. This creates opportunity for lead generators who maintained buyer relationships through AEP and can deliver consistent volume.
OEP Strategic Differences
Consumer psychology differs substantially between AEP and OEP. AEP shoppers are making proactive annual decisions, often comparing multiple options. OEP shoppers are typically dissatisfied with choices made during AEP. Their primary care physician left the network. Prescription costs exceeded expectations. The plan reduced benefits effective January 1.
This dissatisfaction shapes effective messaging. OEP creative should acknowledge the frustration of being in the wrong plan and offer solutions, rather than leading with plan comparisons. Questions like “Is your Medicare Advantage plan working for you?” or “Disappointed with your coverage since January?” resonate with OEP shoppers.
Qualification during OEP requires confirming that the consumer is currently enrolled in a Medicare Advantage plan. Beneficiaries on Original Medicare with standalone Part D are not eligible for OEP changes and represent wasted lead cost if not properly filtered.
Special Enrollment Periods: Year-Round Opportunity
Special Enrollment Periods provide year-round Medicare lead opportunity triggered by qualifying life events. CMS defines numerous SEP triggers that allow beneficiaries to enroll or change coverage outside standard enrollment periods.
Common SEP Qualifying Events
Moving to a new service area where current plan coverage is not available triggers a two-month window to select new coverage. This SEP applies when beneficiaries relocate permanently, not for temporary travel.
Losing employer or union coverage that was creditable creates a 60-day enrollment window. This commonly occurs at retirement when employer-sponsored coverage ends.
Becoming eligible for Extra Help or Low Income Subsidy status allows immediate Part D enrollment and once-per-quarter plan changes.
Leaving a Skilled Nursing Facility creates a brief enrollment window for coverage changes.
Plan termination by CMS when a plan loses its contract creates a mandated SEP.
FEMA-declared disasters trigger SEPs in affected geographic areas.
Chronic Condition Special Enrollment Period
As of 2019, beneficiaries with certain chronic conditions can switch Medicare Advantage plans once per quarter during the first three quarters of the year (January-September). Qualifying conditions include diabetes, cardiovascular disorders, chronic lung disorders, and other specified conditions.
The Chronic Condition SEP creates ongoing lead opportunity for plans specializing in chronic condition management. These plans often offer enhanced benefits for medication management, care coordination, and specialist access that appeal to beneficiaries with qualifying conditions.
5-Star Special Enrollment Period
Beneficiaries can switch to a 5-star rated Medicare Advantage plan at any time throughout the year. This creates year-round opportunity for high-rated plans to acquire members outside enrollment periods.
The 5-star SEP requires lead forms to capture current plan enrollment status and specific interest in 5-star plans. This represents a smaller market segment but with uniquely favorable enrollment timing.
ACA Subsidy Expiration: Market Disruption Risk (December 2026)
The enhanced premium tax credits from the Inflation Reduction Act expire December 31, 2026, creating significant implications for Medicare lead generation.
The Scope of Disruption:
- 22 million of 24 million ACA enrollees receive enhanced subsidies
- Without extension, premiums expected to double or more for many enrollees
- 23.4% average premium spike projected across the exchange market
- 57% of ACA enrollees live in Republican congressional districts
- 80% of premium tax credits ($115 billion) flow to states won by Trump in 2024
Medicare Lead Generation Implications:
T65 Pipeline Impact: Many consumers aging into Medicare during 2026 will have been ACA enrollees who saw dramatic premium increases. This creates heightened awareness of healthcare costs and potentially stronger motivation to optimize Medicare coverage selection.
Market Crossover: Consumers who abandon ACA coverage due to cost may pursue employment specifically for health benefits, delaying Medicare enrollment. Others may accelerate early Medicare enrollment decisions.
Medicare Advantage Positioning: Plans emphasizing low out-of-pocket costs gain additional appeal when consumers have just experienced premium shock in other markets.
Open Enrollment Timing: The 2026-2027 ACA Open Enrollment Period (November 1, 2026 - January 15, 2027) overlaps with Medicare AEP and ends just as the subsidies expire. Expect confused consumers and mixed messaging in the marketplace.
Strategic Response:
- Prepare messaging that addresses premium anxiety from ACA experience
- Train call center teams on ACA-to-Medicare transition questions
- Monitor political developments – subsidy extension remains possible but uncertain
- Segment T65 audiences by prior ACA enrollment status where data permits
SEP Lead Strategy
Year-round Medicare operations must build infrastructure specifically for SEP lead generation. Forms need qualifying event identification. Routing logic needs carriers or agents equipped for SEP enrollment processing. Content and advertising should target life-event triggers rather than general Medicare shopping.
SEP lead pricing typically runs $45-70 for quality exclusive leads year-round, without the dramatic swings of AEP and OEP. Volume is inherently limited by the frequency of qualifying events in the population, but the consistent pricing and less intense competition create opportunity for operators who invest in year-round capability.
CMS Compliance Requirements
The Centers for Medicare and Medicaid Services regulates Medicare marketing with requirements that substantially exceed standard lead generation compliance. Violating CMS rules carries consequences ranging from corrective action plans to Civil Monetary Penalties exceeding $100,000 to complete marketing shutdown. This is not TCPA territory where $500-$1,500 per violation accumulates slowly. CMS can impose immediate operational consequences.
The One-to-One Consent Requirement
CMS implemented one-to-one consent requirements for Medicare marketing in October 2024. This standard is significantly stricter than general TCPA requirements.
Under CMS rules, a Medicare beneficiary must grant explicit consent to be contacted by a specific plan sponsor or Third-Party Marketing Organization. Generic consent to receive Medicare information from “marketing partners” does not satisfy CMS requirements.
The practical implication for lead generation is profound. The standard lead aggregation model where consent is captured once and leads are sold to multiple buyers does not comply with CMS one-to-one consent requirements for Medicare marketing.
Compliant Lead Generation Approaches
Exclusive leads with named disclosure remain fully compliant. The consumer explicitly consents to contact from a specifically named carrier, FMO, or agency. The form clearly identifies the organization that will receive the information and make contact.
Consumer-initiated contact through comparison models where consumers actively select which plans they want information from satisfies the requirement. The consumer controls the distribution by choosing specific plans, creating one-to-one consent for each selected option.
Opt-in to specific plans through form design that allows consumers to select individual plans for contact creates compliant multi-buyer distribution. Each selection represents separate consent.
Real-time transfers provide an exception. When a beneficiary calls a TPMO and can be connected to another organization in real time to provide assistance, prior written consent is not required. However, verbal consent must be obtained and recorded, with the beneficiary explicitly acknowledging the specific organization to which they are being transferred.
Scope of Appointment Requirements
Before any sales appointment, a licensed agent must obtain a completed Scope of Appointment form from the beneficiary. The SOA must be completed at least 48 hours before the appointment, specify which products will be discussed, be signed by the beneficiary, and be retained for 10 years.
Lead Generation Implications
The 48-hour waiting period creates timing considerations that affect lead delivery and buyer follow-up processes. Leads delivered for immediate callback cannot result in product-specific discussions without SOA completion first.
Two common models address this requirement. Some lead generation operations capture digital SOA consent during the form completion process, with the consumer selecting topics for discussion and providing electronic signature before lead delivery. This front-loads SOA completion into lead generation.
Alternatively, leads can be delivered as information requests with agents responsible for SOA completion before any appointment. Initial contact is limited to fact-finding without product recommendations, with formal appointments scheduled after SOA completion and the 48-hour waiting period.
Exceptions to the 48-Hour Rule
Beneficiary-initiated contact where the beneficiary specifically requests immediate assistance can proceed without the waiting period. Marketing events where attendees complete SOA at the event allow same-day discussion. Appointments where agents provide only general plan information without specific recommendations do not require SOA.
Prohibited Marketing Practices
CMS explicitly prohibits numerous practices that are common in other lead generation verticals:
Unsolicited contact of any kind without prior consent is prohibited. This includes door-to-door, telephonic, and electronic contact. Cold calling beneficiaries is never permitted.
Marketing at healthcare provider offices, pharmacies, or other healthcare settings is prohibited.
Cross-selling non-health products during Medicare presentations violates CMS rules. An agent cannot discuss life insurance or annuities during a Medicare sales appointment.
Gifts exceeding the CMS-established nominal value limit (currently $15 retail value) are prohibited as marketing incentives.
Conducting sales activities at educational events is prohibited. Educational events must remain purely educational without any sales closing.
Misleading plan comparisons or guarantees of enrollment outcomes create enforcement risk.
Civil Monetary Penalties
CMS penalties for marketing violations can reach $100,000 or more per violation. Unlike TCPA where violations accumulate at $500-$1,500 each before reaching significant totals, a single CMS violation can create six-figure liability.
Beyond financial penalties, CMS can impose intermediate sanctions including suspension of enrollment, marketing material approval suspension, or termination from Medicare program participation. For carriers and FMOs, program termination represents existential risk.
CMS increased enforcement actions in 2024, particularly targeting deceptive advertising and consent violations involving Third-Party Marketing Organizations.
CPL Benchmarks by Medicare Lead Type
Medicare lead pricing varies based on lead type, qualification level, and enrollment period timing. Understanding accurate benchmarks prevents overpaying for leads and helps set realistic expectations for lead generation economics.
Medicare Advantage Leads
Medicare Advantage (Part C) leads represent the highest-volume Medicare lead type. MA plans bundle hospital coverage (Part A), medical coverage (Part B), and usually prescription drug coverage (Part D), often with additional benefits including dental, vision, hearing, and fitness programs.
CPL Ranges by Quality Tier
Basic Medicare Advantage leads with minimal qualification and potential OEP or SEP eligibility uncertainty typically price at $30-45.
Qualified Medicare Advantage leads with confirmed AEP eligibility and current coverage verification command $50-70.
Premium Medicare Advantage leads including completed health questionnaires and specific plan interest indication reach $70-100.
Live transfers with agent-to-agent warm handoff of pre-qualified beneficiaries price at $100-175, sometimes exceeding $200 for transfers meeting specific demographic and geographic criteria.
Seasonality Impact
AEP pricing runs 30-50% above baseline. Early AEP (October 15-31) commands premium pricing as carriers front-load campaigns. Late AEP (November 15-December 7) often sees price compression as carriers approach enrollment targets or exhaust allocated budgets.
Medicare Supplement Leads
Medicare Supplement policies (Medigap) fill gaps in Original Medicare coverage. Unlike Medicare Advantage, Medigap policies are sold by private insurers and require separate premium payments in addition to Part B premiums.
CPL Ranges by Quality Tier
Basic Medigap leads indicating interest with basic demographics price at $45-60.
Qualified Medigap leads with current coverage confirmation and plan comparison interest reach $60-85.
Premium Medigap leads including health history and specific plan type preference (Plan F, Plan G, Plan N) command $85-110.
Key Consideration: Open Enrollment Timing
Medigap leads maintain year-round value because Medicare Supplement Open Enrollment differs from MA enrollment periods. Beneficiaries have a one-time, six-month Medigap Open Enrollment Period that begins when they are both age 65 or older and enrolled in Part B.
During this window, insurers must accept applicants without health underwriting. Outside this window, applicants face medical underwriting that can result in higher premiums, benefit waiting periods, or denial of coverage (except in states with guaranteed-issue requirements).
T65 Medigap leads command premium pricing specifically because these beneficiaries are within their guaranteed-issue window.
Part D Prescription Drug Leads
Standalone Part D leads represent the lowest CPL tier in Medicare. Many beneficiaries handle Part D enrollment themselves or receive prescription coverage through Medicare Advantage or employer plans.
Basic Part D leads indicating interest in prescription coverage price at $20-35.
Qualified Part D leads with current medications documented reach $35-50.
Premium Part D leads identifying formulary concerns or specific drug cost issues command $50-65.
The lower CPLs reflect lower commission values for Part D sales. Many agents pursue Part D leads as entry points for Medicare Advantage cross-sell opportunities during future enrollment periods rather than as standalone revenue opportunities.
Live Transfer and Warm Transfer Leads
Live transfers represent the premium tier of Medicare leads. These are phone calls where a call center agent has pre-qualified the beneficiary and transfers them directly to a licensed sales agent while the consumer remains on the line.
Live Transfer Pricing Factors
Call duration minimums affect pricing. Transfers requiring minimum call lengths of 60 or 90 seconds before billing command higher prices.
Qualification depth including health questions answered, current coverage verified, and specific plan interest established creates premium pricing.
Transfer timing affects economics. Immediate transfers command different pricing than scheduled callback transfers.
Exclusivity determines whether single agents receive transfers or whether multiple agents compete.
Geographic targeting creates regional pricing variation based on carrier availability and plan richness.
Live Transfer Economics
The higher CPL for live transfers often delivers better unit economics despite the price premium. A $125 live transfer converting at 15% delivers cost per acquisition of $833. A $50 data lead converting at 4% delivers cost per acquisition of $1,250. The math frequently favors live transfers for operations prioritizing efficiency over volume.
Qualifying the Senior Demographic
Medicare lead generation requires different qualification approaches than younger demographics. Understanding senior communication preferences, technology comfort levels, and decision-making patterns improves both lead quality and conversion rates.
Senior Communication Preferences
Phone remains the dominant sales channel for Medicare. Research consistently shows that 60-75% of seniors prefer phone contact over email or digital communication for insurance decisions, with preferences varying by age within the 65+ population.
This creates operational implications. Phone number validation carries elevated importance in Medicare lead generation. Email-only leads have limited value because the conversion path runs through phone contact regardless of initial capture method.
Landing pages targeting Medicare consumers should prominently feature phone numbers for those who prefer calling directly rather than completing forms.
Form Design for Senior Users
Medicare forms must accommodate users who may have vision limitations, lower technology familiarity, or different interaction patterns than younger consumers.
Font sizes should meet minimum thresholds of 16 pixels, with 18 pixels preferred for body text. Form labels and error messages should match these standards.
High contrast between text and backgrounds improves readability. Black text on white backgrounds performs better than gray text or colored backgrounds with subtle contrast.
Simple single-column layouts with generous whitespace reduce cognitive load. Avoid multi-column layouts that create reading pattern confusion.
Large click targets meeting minimum dimensions of 44x44 pixels reduce frustration from missed taps on mobile devices or imprecise cursor placement on desktop.
Clear error messages and progress indicators help users understand where they are in multi-step forms and what corrections are needed when validation fails.
Phone support options as alternatives to form completion capture prospects who abandon digital forms due to difficulty or preference for human interaction.
Device Considerations
Medicare audiences skew toward desktop usage compared to younger demographics. Desktop traffic represents 45-55% of Medicare form submissions, compared to 25-35% for auto insurance or solar leads where mobile dominates.
This pattern reflects both generational technology adoption and decision-making context. Seniors comparing Medicare options often use larger screens that allow easier reading of plan details and comparison across multiple sources.
Desktop optimization matters more for Medicare than for other insurance verticals. Ensure forms render well on larger screens and that landing pages take advantage of available screen real estate rather than being mobile-only designs stretched to desktop dimensions.
Qualification Questions That Improve Lead Quality
Medicare lead qualification requires specific questions that determine eligibility, enrollment period, and purchase intent.
Essential Qualification Fields
Age or date of birth determines Medicare eligibility. Under-65 leads without disability indicators represent wasted cost unless specifically targeting the disabled population.
Current Medicare status identifying whether the prospect has Original Medicare, Medicare Advantage, or has not yet enrolled determines which products are relevant and which enrollment periods apply.
Part A and Part B enrollment status matters because both are required for Medicare Advantage enrollment. Beneficiaries with Part A only cannot enroll in MA plans.
ZIP code determines available plans since Medicare Advantage and Part D plan availability varies by county.
Contact preference captures preferred communication method and best contact times. Seniors often have specific availability windows and strong preferences.
Enhanced Qualification Fields for Higher-Value Leads
Current monthly premium indicates price sensitivity and potential savings opportunity.
Primary care physician name and address determines network compatibility for Medicare Advantage plans.
Current prescription medications allow formulary matching and drug cost comparisons.
Health conditions including chronic conditions trigger Chronic Condition SEP eligibility and determine D-SNP (Dual Eligible Special Needs Plan) potential.
Dual eligibility status identifying beneficiaries with both Medicare and Medicaid opens D-SNP enrollment opportunities.
Expected qualifying event for leads captured outside AEP/OEP establishes SEP eligibility.
Quality Indicators and Red Flags
Certain patterns indicate low-quality or potentially fraudulent Medicare leads:
Age under 65 with no disability indicator suggests either data error or fraudulent submission.
ZIP codes in territories without Medicare Advantage plans represent either fake data or extremely limited buyer demand.
Phone numbers with repeated digits, sequential patterns, or area codes mismatched to stated locations indicate potential fraud.
Form completion times under 30 seconds on multi-question forms suggest bot activity or incentivized form filling.
Multiple submissions from the same IP address within short time periods indicate incentive fraud.
Email addresses created immediately before form submission or containing random character strings suggest fake leads.
Working with FMOs and Direct Carriers
Medicare lead buyers fall into two primary categories: Field Marketing Organizations and direct carriers. Understanding each buyer type affects lead pricing, volume requirements, and relationship dynamics.
Field Marketing Organizations
FMOs serve as intermediaries between insurance carriers and independent agents. They provide contracting relationships, training, compliance support, marketing resources, and lead distribution to their agent networks.
FMOs purchase leads in bulk for redistribution. Volume requirements typically start at 500-1,000 leads monthly for meaningful relationships, with larger FMOs absorbing 5,000+ leads monthly during AEP.
Geographic routing matters because FMOs distribute leads to agents based on territory. Lead generators serving FMOs need either national coverage or explicit agreements about geographic focus.
Buying concentration occurs heavily during AEP. Many FMOs purchase 70-80% of annual lead volume during the October-December window, with reduced or paused purchasing during Q2-Q3.
FMO relationships offer faster ramp-up, more flexibility on volume requirements, and often shorter sales cycles (weeks rather than months). Payment terms typically run 30-45 days.
The tradeoff involves pricing pressure from bulk purchasing and less per-lead revenue compared to direct carrier relationships.
Direct Carrier Relationships
Large Medicare carriers including UnitedHealthcare, Humana, Aetna, Cigna, and Anthem maintain internal lead acquisition operations and work with external lead generators.
Carrier relationships involve CMS-driven compliance requirements that exceed FMO standards. Carriers face direct regulatory scrutiny and transfer that scrutiny to lead sources.
Geographic targeting follows plan availability. Carriers want leads in counties where they offer competitive plans, not nationwide distribution that includes unprofitable territories.
Volume requirements are substantial, typically 3,000-5,000 leads monthly minimum for direct relationships, with some carriers requiring 10,000+ monthly during AEP.
Carrier sales cycles run 6-12 months for initial relationship establishment, with extensive compliance audits before lead flow begins.
The advantages include higher per-lead pricing, more stable demand, and longer-term contracts. Payment reliability is typically excellent given carrier financial strength.
Building a Balanced Buyer Portfolio
Successful Medicare lead operations diversify across buyer types:
40-50% direct carrier relationships provide stability, premium pricing, and predictable year-over-year demand.
30-40% large FMO relationships offer volume absorption and flexibility when carrier caps fill.
10-20% regional agents and smaller FMOs allow relationship testing, provide pricing benchmarks, and create backup demand.
This distribution protects against single-buyer dependency while maintaining negotiating leverage through demonstrated ability to route volume to alternatives.
T65 Lead Generation Strategies
T65 leads represent prospects approaching their 65th birthday who are making Medicare decisions for the first time. This segment commands premium pricing and requires specific targeting strategies.
Why T65 Leads Command Premium Pricing
Several factors combine to make T65 leads the highest-value Medicare segment:
First-time decision-making creates receptivity to guidance. Unlike beneficiaries who have been on Medicare for years and have established preferences, T65 prospects are learning the system from scratch.
Guaranteed-issue Medigap windows apply. During the six-month period starting when beneficiaries are both 65+ and enrolled in Part B, they can purchase any Medicare Supplement policy regardless of health status. This window creates urgency and value.
Longer customer lifetime translates to higher lifetime value. A 65-year-old enrolled beneficiary represents more years of potential renewal commissions than someone enrolling at 70 or 75.
Multiple product opportunities exist. T65 prospects need decisions on Medicare Advantage versus Original Medicare plus Medigap, Part D coverage if choosing Original Medicare, and potentially dental, vision, and other ancillary products.
T65 CPL Benchmarks
Basic T65 leads with age verification and contact information price at $55-75.
Qualified T65 leads with current insurance status, retirement timeline, and Medicare readiness indication reach $80-120.
Premium T65 leads within 90 days of 65th birthday with confirmed Part B enrollment timing command $120-175.
T65 live transfers with pre-qualification exceed $150-225.
Timing T65 Lead Generation
The Initial Enrollment Period for Medicare spans seven months: three months before the beneficiary turns 65, the month of their 65th birthday, and three months after.
Effective T65 targeting follows a timeline approach:
6-12 Months Before 65th Birthday
Early awareness campaigns build familiarity and capture email addresses for nurture sequences. Content at this stage should be educational, explaining what Medicare is, how it differs from employer coverage, and what decisions lie ahead.
Lead value at this stage is lower ($40-60) because purchase timing is distant. However, capturing early allows nurture campaigns that build relationship before the decision window.
4-6 Months Before 65th Birthday
Active research phase begins. Prospects start comparing options, understanding plan types, and considering their preferences. Comparison tools, decision guides, and specific product information become relevant.
Lead values increase to $60-90 as purchase timing approaches.
1-3 Months Before 65th Birthday
The Initial Enrollment Period opens. Prospects need to make decisions about Part B enrollment timing, plan selection, and coverage start dates. This represents highest value and highest urgency.
Lead values reach $100-150+ as immediate conversion opportunity exists.
Birthday Month
Peak urgency for coverage start date decisions. Prospects who have not yet enrolled face immediate choices about when coverage begins.
1-3 Months After 65th Birthday
Late IEP opportunity for prospects who delayed decisions. After this window closes, enrollment options become more limited.
T65 Data Sources and Targeting
Multiple data sources enable T65 targeting:
Voter registration files contain date of birth information that can be modeled for T65 timing.
DMV records, where available, provide age data for targeting.
Consumer data compilers including Experian, Acxiom, and similar providers offer T65 audiences based on age and demographic modeling.
Facebook and Meta platforms support age-based targeting for Medicare advertising, though with restrictions that require compliance review.
Google Ads allows age targeting that can reach T65 audiences through search and display campaigns.
T65 Targeting Recommendations
Begin awareness targeting 6-9 months before 65th birthdays to build familiarity.
Concentrate conversion-focused spending 3-4 months before birthday when research activity peaks.
Apply geographic targeting based on carrier plan availability and lead buyer demand.
Consider income targeting for Medigap campaigns since higher-income beneficiaries more often choose Original Medicare plus Medigap over Medicare Advantage.
T65 Messaging Approaches
Effective T65 messaging themes include:
Transition guidance emphasizing help navigating the change from employer coverage to Medicare.
Timeline urgency without panic, explaining enrollment windows and consequences of missing them.
Guaranteed-issue emphasis for Medigap opportunities, noting the limited window for health-status-irrelevant enrollment.
Simplification of complex choices, positioning the brand as a guide through confusing options.
Messaging to Avoid
Fear-based messaging about Medicare complexity creates resistance rather than engagement.
Pushy sales language conflicts with senior communication preferences for relationship-based decision making.
Promises of “free” coverage without qualification around income or geographic limitations create compliance risk.
Compliance Infrastructure and Risk Management
CMS enforcement intensity increased substantially in 2023-2026. Building compliance into operations from the beginning protects against enforcement actions and positions operations for sustainable buyer relationships.
Building Compliant Lead Generation Operations
Lead generation compliance requires integration across form design, consent capture, documentation, and buyer contracts.
Form and Creative Compliance
All advertising materials require review for prohibited claims. Medicare advertising cannot promise specific benefits that vary by geography or make claims about coverage without appropriate disclaimers.
Consent language must specifically comply with CMS one-to-one consent requirements. Generic consent covering “marketing partners” is insufficient.
Consent capture must include timestamp, IP address, and specific documentation of what the consumer saw and agreed to.
Creative approval through CMS is required for materials used by TPMOs. The 30-45 day approval timeline requires advance planning for enrollment period campaigns.
Documentation and Retention
Consent documentation should be retained for CMS-required periods, typically 10 years for materials related to enrollment decisions.
Call recordings for any telephone contact with beneficiaries should be retained with clear organization for retrieval if compliance questions arise.
Form versions, consent language changes, and creative updates should be tracked with effective dates for audit defensibility.
Buyer Contracts
Contracts with carriers and FMOs should include compliance representations about lead generation methods.
Understanding buyer compliance requirements before lead flow begins prevents post-facto disputes about whether leads meet buyer standards.
Regular communication about compliance changes at either the CMS level or within buyer organizations maintains relationship health.
Common Compliance Failures
Lead generation operations most commonly fail on consent documentation, benefit misrepresentation, contact timing, and cross-selling boundaries.
Consent Documentation Failures
Form language not specifically naming plan sponsors or providing individual selection.
Consent captured without proper timestamp and IP documentation.
Consent language buried in terms of service rather than presented as clear, conspicuous disclosure.
Missing E-SIGN disclosure requirements for electronic consent.
Benefit Misrepresentation
Claims like “$0 premium Medicare Advantage” without geographic disclaimers.
Promises about specific benefits that may not be available in all plans or areas.
Comparison claims that do not reflect actual plan differences.
Contact and SOA Timing
Agents discussing specific plan recommendations before SOA completion and 48-hour waiting period.
Initial contact positioned as sales conversation rather than fact-finding.
Failure to document SOA completion and timing.
Cross-Selling Boundaries
Introducing non-Medicare products during Medicare presentations.
Agents offering life insurance, annuities, or other products during Medicare enrollment appointments.
Seasonality and Budget Planning
Medicare lead generation economics vary dramatically by season. Effective budget planning requires understanding enrollment period patterns and allocating resources accordingly.
Monthly Demand Patterns
January: OEP begins. Moderate-to-high demand from Medicare Advantage plan changers. Post-AEP carryover from December creates continued activity.
February-March: OEP continues through March 31. Steady demand at moderate levels.
April-May: Off-season begins. Demand drops to SEP-only levels. Lead prices soften 25-40% from AEP peaks.
June-July: Low demand. T65 targeting provides most consistent volume. Smart practitioners use this period to test creative and landing pages at lower cost.
August-September: Pre-AEP preparation accelerates. Carriers and FMOs finalize plan offerings and lead contracts. Buyers begin testing lead sources for AEP capacity.
October: AEP begins October 15. Demand shifts to maximum levels within days. Premium pricing applies throughout the month.
November: Peak AEP demand continues. November 15 represents effective midpoint for enrollment decisions. Budget exhaustion at some buyers creates spot opportunities with others.
December: AEP ends December 7. Concentrated last-week demand from deadline-driven enrollees. Post-December 7, demand drops immediately to OEP anticipation levels.
Budget Allocation Strategy
A $100,000 annual Medicare lead generation budget might be allocated as follows:
AEP (October 15 - December 7): 40-45% of annual budget. This concentrated investment captures the majority of annual value during the highest-demand period.
OEP (January 1 - March 31): 20-25% of annual budget. Secondary peak with more moderate pricing.
Year-round SEP and T65: 25-30% of annual budget. Consistent base operation maintaining buyer relationships and capturing ongoing qualifying event volume.
Testing and reserve: 5-10% of annual budget. Creative testing during low-demand periods and reserve for AEP overperformance that justifies additional investment.
Scaling Considerations
Medicare lead generation faces specific scaling challenges:
Seasonal inventory constraints limit how much quality traffic is available during enrollment periods regardless of budget.
Buyer capacity limits create caps that may fill before available budget is exhausted.
Compliance overhead scales with volume, requiring additional quality assurance, documentation management, and buyer communication.
Geographic limitations from plan availability restrict addressable markets for specific carrier buyers.
Frequently Asked Questions
What is the difference between Medicare Advantage and Medicare Supplement leads?
Medicare Advantage (Part C) leads are for beneficiaries interested in all-in-one plans that replace Original Medicare with coverage from private insurers. Medicare Supplement (Medigap) leads are for beneficiaries who want to keep Original Medicare but add coverage for out-of-pocket costs like copays, coinsurance, and deductibles. The enrollment rules differ substantially: MA follows AEP/OEP/SEP periods, while Medigap has guaranteed-issue periods tied to Part B enrollment. Lead economics differ as well, with Medigap leads typically pricing 15-30% higher than comparable MA leads.
Can I sell Medicare leads to multiple buyers like in other verticals?
CMS one-to-one consent requirements, effective October 2024, restrict traditional shared lead models in Medicare. Beneficiaries must consent to contact from specific plan sponsors or TPMOs. Compliant approaches include exclusive leads with named disclosure, consumer-selection comparison models where beneficiaries actively choose which plans to hear from, or separate consent capture for each potential buyer. Multi-buyer distribution without specific consent for each buyer creates CMS enforcement risk.
What CPL should I expect for Medicare Advantage leads during AEP?
During the Annual Enrollment Period (October 15 - December 7), Medicare Advantage lead CPLs typically range from $60-100 for qualified leads, compared to $40-60 during off-season periods. Premium leads with full qualification, health questionnaire completion, and specific plan interest regularly exceed $100. Live transfers during AEP range from $120-200+. Pricing varies by geographic target, qualification depth, and buyer capacity availability.
How do I generate Medicare leads year-round outside of AEP?
Year-round Medicare lead generation focuses on Special Enrollment Periods triggered by qualifying life events (moving, losing employer coverage, gaining Medicaid eligibility), T65 prospects approaching their Initial Enrollment Period, and Medicare Supplement leads which follow different enrollment rules. The Chronic Condition SEP allows quarterly plan changes for beneficiaries with qualifying conditions. Content marketing targeting these segments provides consistent year-round volume at stable pricing.
What is a Scope of Appointment and why does it matter for lead generation?
A Scope of Appointment is a CMS-required document that must be completed at least 48 hours before a sales appointment discussing specific Medicare products. The SOA specifies which product types will be discussed and protects beneficiaries from unwanted sales pressure. Lead generators must understand SOA requirements because they affect how leads can be contacted and what conversations can occur during initial outreach. Leads delivered for immediate callback cannot result in product-specific discussions without SOA completion and 48-hour waiting period.
Are live transfer Medicare leads worth the premium price?
Live transfer leads typically cost $100-200+ compared to $40-100 for data leads, but conversion rates are often 3-5x higher. A $150 live transfer converting at 15% delivers an $1,000 cost per acquisition. A $60 data lead converting at 4% delivers a $1,500 cost per acquisition. The math often favors live transfers despite higher per-lead costs, particularly for operations prioritizing efficiency over volume. Live transfers also provide immediate engagement without the contact rate challenges that affect data lead performance.
What compliance risks are unique to Medicare lead generation?
Medicare lead generation carries CMS compliance requirements beyond standard TCPA obligations. Key risks include one-to-one consent violations (requiring specific plan sponsor identification rather than generic marketing consent), Scope of Appointment failures (product discussions before SOA completion and 48-hour waiting period), misleading benefit claims (promising coverage that varies by geography or plan), prohibited cross-selling (introducing non-Medicare products during Medicare presentations), and inadequate documentation retention (CMS requires 10-year retention for enrollment-related materials). CMS can impose Civil Monetary Penalties exceeding $100,000 per violation.
How do I target T65 (Turning 65) prospects effectively?
T65 targeting uses age-based data from voter files, DMV records, and consumer data compilers. Begin awareness campaigns 6-9 months before birthdays to build familiarity and capture email addresses for nurture. Concentrate conversion-focused spending 1-4 months before eligibility when research activity and purchase intent peak. Facebook and Google both support age-based targeting for Medicare advertising with appropriate compliance considerations. T65 leads command premium pricing ($80-175 depending on qualification and timing proximity) due to guaranteed-issue Medigap rights and first-time decision-making opportunity.
Should I work with FMOs or try to sell directly to carriers?
Most successful Medicare lead operations work with both buyer types. Direct carrier relationships offer premium pricing and year-over-year stability but require significant volume commitments (3,000-10,000+ leads monthly) and longer sales cycles (6-12 months for initial relationship). FMOs offer faster ramp-up, smaller minimum volumes, and more geographic flexibility but typically pay less per lead. A diversified portfolio with 40-50% carrier relationships, 30-40% large FMO relationships, and 10-20% regional or smaller buyers provides optimal balance between pricing and flexibility.
What makes Medicare lead forms different from other insurance verticals?
Medicare forms must accommodate senior users with accessibility considerations: larger fonts (minimum 16px, preferably 18px), high contrast design, simple single-column layouts, large click targets (minimum 44x44 pixels), and clear error messages with progress indicators. Phone number validation is critical because phone remains the dominant sales channel for Medicare. Desktop optimization matters more than in other verticals since seniors use desktop devices 45-55% of the time compared to 25-35% in younger demographics. Forms should capture Medicare-specific qualification data including current coverage status, Part A and B enrollment, ZIP code for plan availability determination, and preferred contact times.
Key Takeaways
Enrollment periods determine strategy. AEP (October 15 - December 7) drives 60-70% of annual Medicare lead value. Budget allocation, creative preparation, and buyer relationships must be planned around this 54-day window. OEP (January 1 - March 31) provides secondary opportunity, while year-round SEP and T65 leads require dedicated infrastructure.
CMS compliance exceeds TCPA standards. One-to-one consent requirements, Scope of Appointment rules, 48-hour waiting periods, and prohibited marketing practices create a compliance environment that demands purpose-built processes. Civil Monetary Penalties exceeding $100,000 per violation make compliance infrastructure essential, not optional.
CPL benchmarks vary substantially by lead type and timing. Medicare Advantage leads range from $40-100+ depending on qualification depth and enrollment period timing. T65 leads command premiums of $80-175. Live transfers range $100-200+ but frequently deliver better cost-per-acquisition than data leads despite higher per-lead pricing.
The senior demographic requires adapted approaches. Form design, communication preferences, and decision-making patterns differ from younger demographics. Larger fonts, simpler layouts, phone-first contact strategies, and patience in communication improve both lead quality and conversion outcomes.
Buyer diversification protects revenue. Balance direct carrier relationships providing stability and premium pricing with FMO relationships offering volume absorption and flexibility. Single-buyer dependency creates existential risk when that buyer reduces capacity or changes requirements.
T65 leads represent the premium segment. First-time Medicare decisions, guaranteed-issue Medigap windows, and longer customer lifetimes make T65 the highest-value opportunity. Target 6-9 months before 65th birthdays for awareness, concentrate conversion investment 1-4 months before eligibility.
Compliance infrastructure scales with volume. Documentation, quality assurance, and buyer communication requirements increase as lead volume grows. Build compliance into operations from the beginning rather than attempting to retrofit after CMS scrutiny arrives.
Statistics and regulatory information current as of late 2025. CMS updates Medicare Communications and Marketing Guidelines annually, and enrollment period economics shift based on plan offerings and carrier competition. Verify current compliance requirements before acting on any regulatory claims.